Prostate Cancer
WHAT MEN OVER 40 SHOULD KNOW

Robert Nam, winner of the
George Armstrong-Peters Prize
|
Recently a large randomized
trial demonstrated a significant
20% reduction in prostate
cancer mortality among
patients who underwent prostate
cancer screening with
a blood test called prostate
specific antigen (PSA) (1). This
finding coupled with another
randomized trial demonstrating
men undergoing radical
prostatectomy versus watchful
waiting had a 50% reduction in prostate cancer mortality
would seem to suggest the pathway for success in
prostate cancer is clear: screen aggressively with PSA and
treat aggressively with surgery (2). However, as Dr. Nam
points out, the solution may not be that clear.
PSA is not an ideal biomarker for screening. Initially
after its inception in 1987 it was very effective. The
'cutoff ' of normal PSA at 4 ng/mL identified many of
the men who were harbouring prostate cancer for years.
However, since that harvest period, we've learned that
prostate cancer is still prevalent even at low PSA values.
The majority of cancers detected in 2009 occur in men
with PSAs below 4.0 ng/mL.
Simply lowering the cutpoint for a normal PSA would
certainly capture more prostate cancers, however it
would mean many more men would undergo prostate
biopsy in order to find these cancers. In his study of
Ontario-wide data, Dr. Nam found the rate of complications
after prostate biopsy is increasing, perhaps due
to the increasing prevalence of drug-resistant bacterial
strains. In 2006, 4% of men undergoing a prostate biopsy
were subsequently admitted to hospital with sepsis,
compared to 1% in 1996.
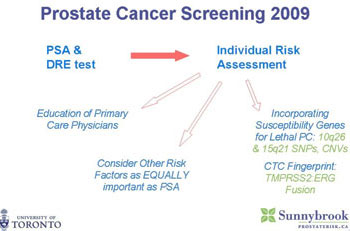
Given this screening conundrum, Dr. Nam suggests the
medical community needs more refined 'selective screening'
and prostate cancer genetic markers may help. He
has worked extensively in developing a better screening
instrument that incorporates PSA and other risk factors
and tumour markers for prostate cancer. He developed
a prostate cancer risk calculator that performs better
than PSA alone. There have been several gene markers
that have been associated with prostate cancer. A recent
study demonstrated 5 single-nucleotide polymorphisms
(SNPs) were strongly associated with prostate cancer (3). A
man possessing all 5 SNPs has 9 times the risk of being
diagnosed with prostate cancer compared to those without
any of the 5 SNPs. In breast cancer our understanding
of these genes is profound enough to make clinical
decisions (e.g. offering prophylactic mastectomy for
carriers of the BRCA-1 mutation); our understanding of
genes in prostate cancer is not mature enough yet. For
example, we don't know the biological function of the
actual genes in which these SNPs reside; the predictive
value of using the SNPs is not that much greater than
our current conventional risk factors (age, family history,
rectal exam and PSA); and the SNPs do not help delineate
those harbouring high grade aggressive tumours.
|
The ability to distinguish those with high grade tumours
versus those with low grade tumours is the key issue
in prostate cancer. Those with high grade tumours
are much more likely to die from prostate cancer. Dr.
Nam has taken the concept of using genetic markers
one step further. Using state of the art Genome Wide
Associations Studies (GWAS) he identified several new
SNPs associated in particular with high grade tumours.
These SNPs at 10q26 and 15q21 are significantly
associated with aggressive forms of prostate cancer.
Prostate Cancer Screening 2009
|
Combinations of these risk alleles were found to have a
3-fold increase in risk for aggressive prostate cancer. This
is the first time SNPs have been found to be predictive
of high grade prostate cancer. In a related research pathway,
Dr. Nam is studying what happens when two genes,
TMPRSS2 and ERG, fuse in a variable way. Variants in
the TMPRSS2:ERG fusion transcript have been associated
with prostate cancer, and in particular progression
of cancer after surgical treatment. If TMPRSS2:ERG is
identified in circulating tumour cells of men who present
for screening, then they are at substantially increased
risk of having an aggressive form of prostate cancer.
In summary, Dr. Nam feels we must work towards more
selective screening and selective treatment to better
identify men who will benefit from prostate biopsy and
radical treatment of their cancer. This selective screening
must begin with educating the primary care physicians
to identify men at risk. Then an individual risk assessment
must be done using traditional risk factors and
eventually incorporating susceptibility genetic markers
like the SNPs and circulating tumour cell profiles to
maximize the yield of men undergoing prostate biopsy
in hopes of identifying early those with high risk prostate
cancer.
Robert Hamilton
PGY-5, Urology
- Schroder FH, Hugosson J, Roobol MJ, et al. Screening
and prostate-cancer mortality in a randomized European
study. N Engl J Med 2009;360(13):1320-8.
- Bill-Axelson A, Holmberg L, Ruutu M, et al. Radical prostatectomy
versus watchful waiting in early prostate cancer.
N Engl J Med 2005;352(19):1977-84.
- Zheng SL, Sun J, Wiklund F, et al. Cumulative association
of five genetic variants with prostate cancer. N Engl J Med
2008;358(9):910-9.
|