"How Should We Treat Gastric Cancer?"
 Natalie Coburn
|
Surgical oncologist Natalie
Coburn from the Division
of General Surgery and
Sunnybrook Health Sciences
Centre hosted an expert panel
on Processes of Care of Gastric
Cancer on Oct. 21-23rd at the
Four Seasons Hotel in Toronto.
Sixteen experts from six countries
specializing in Medical,
Radiation and Surgical
Oncology, Minimal Access and
General Surgery, and Gastroenterology participated.
A Rand UCLA appropriateness method was used to
organize the meeting. The panelists had scored 2000
scenarios and formulated optimal management strategies
for the surgical treatment of gastric cancer.
As background, Natalie first completed a literature
review on the outcome of treatment of gastric cancer.
The results of surgery are highly variable, and remarkably better in the Eastern hemisphere than in the West.
Asian surgeons tend to overwhelmingly favour D2 resections,
illustrated in a nearby figure, whereas Western
surgeons, influenced by the high mortality reported in
earlier randomized trials, tend to treat the disease less
radically. The evidence base for more limited surgery
comes from earlier randomized trials in which the postoperative
mortality was 10% or more for D2 resections.
Proponents of the D2 operation point out that the
randomized trials included low volume surgeons with a
higher than average mortality.
In the convened expert panel discussion, Dr. Sung Hoon
Hoh, a senior surgeon from South Korea, stated that
he personally performs 500 gastric cancer resections
per year, approximately the same number that are performed
annually in all of Ontario. The panel agreed that
technically challenging minimally invasive resections
should not be endorsed unless performed by surgeons
with advanced laparoscopic skills and extensive experience
in the treatment of gastric cancer. The panel did
not endorse resection of the stomach in the presence of
metastatic disease unless necessary for palliative reasons.
Gastroenterologist Norman Marcon from St. Michael's
Hospital discussed mucosal resections for the earliest
lesions, and this was endorsed by the panel. In general,
treatment of other gastric cancers by surgery alone was
judged to be insufficient. Perioperative chemotherapy or
postoperative chemo-radiation treatment were endorsed
for all gastric cancers more extensive than T1 N0 lesions.
The application of known effective adjuvant treatment
is very much dependent on choices made by the various
treatment teams. The addition of perioperative chemotherapy
raises the five-year survival from 23% to 36%,
and adjuvant chemoradiation increased median survival
from 27 to 36 months.
|
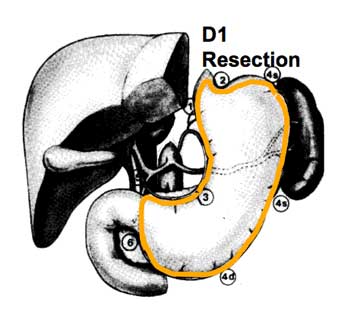 D1 LN dissection: right cardial, left cardial, along lesser curvature, along greater curvature, along gastroepiploics, suprapyloric, infrapyloric; all nodes within 3 cm of primary tumour
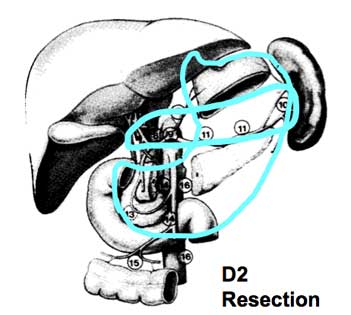 D2 LN dissection: left gastric artery, common
hepatic artery, celiac axis, splenic hilum,
splenic artery; all nodes more than 3 cm
away from primary as well as along the common
hepatic, splenic and L gastric artery
The next step in this important translational research
is development of an education program based on outcomes,
followed by a study of the program's impact on
patients treated for gastric cancer in Ontario. This is the
next iteration of the outstanding translational research
and education program championed by the Sunnybrook
group for treatment of colon cancer patients.
Natalie took her surgical training at Brown University,
completed a fellowship in Surgical Oncology at the
University of Toronto, and has joined Andy Smith and
his colleagues at SHSC and the Odette Cancer Centre,
where she specializes in hepatobiliary and upper GI
cancer. She conducted her studies under a grant from
the Canadian Cancer Society Research Institute and a
Ministry of Health Career Scientist Award.
M.M.
|