First Annual Balfour Lecture
in Surgical Ethics
“ MISTAKES HAVE CHANGED: 40 YEARS
OF WATCHING SURGEONS CREATE
ACCOUNTABILITY”

Donald Balfour
|
Donald Church Balfour,
1882 – 1963, received his
MD from the University
of Toronto, interned at
Hamilton City Hospital,
and studied surgery at the
Mayo Clinic. His father
was president of the
Balfour Tool Company.
Donald devised and introduced numerous instruments
– an operating table, operating room mirror
for teaching, an abdominal retractor. He married
Carrie, Will Mayo’s daughter, and spent his distinguished
career at the Mayo Clinic. He became
Chief of General Surgery and President of the
Mayo Foundation for Education and Research. He
received many honors and awards as a surgical educator
and scholar. His family endowed the annual
Balfour Lecture that celebrates his memory and
brings distinguished scholars in Surgical Ethics to
teach in our Department.
|

Charles Bosk
|
Charles Bosk is a distinguished
social scientist and a careful student
of the tribal customs, values,
and beliefs of surgeons. His
doctoral thesis in sociology was
based on 18 months of ethnographic
observation as an active
member of the surgical team
at the University of Chicago.
His publication “Forgive and
Remember: Managing Medical Failure” became a classic of the sociology and surgical literature.
(The following paragraphs are the Editor’s approximations
of direct quotations. They are not verbatim)
Professor Bosk’s areas of specialization as a medical
sociologist include professions and professionalization,
deviance and social control, field methods of research,
and the sociology of bioethics. He has three ongoing
funded research projects: 1) how ideas about safety move
from national policy-setting bodies formulate ideas about
‘safety’ that then move into administrative offices of hospitals
where they are converted into policies that are then
embraced or evaded on the floors where care is provided;
2) an ethnographic exploration of mandated duty hour
limits on graduate medical education, especially as it
impacts patient care and definitions of
professionalism; and 3) an intervention to
mitigate chronic fatigue in medical residents
through a mandatory nap program.
He is the author of “What Would You
Do?: Juggling Bioethics and Ethnography”;
“All God’s Mistakes: Genetic Counseling
in a Pediatric Hospital”; “Forgive and
Remember: Managing Medical Failure”;
and is currently working on a manuscript
“Thirteen Ways of Looking at a Medical
Error.”
“Administrative rhetoric shapes and
misconstructs the issue of surgical error.
The analogy to airline crashes is a very
poor fit that misleads our thinking. If the
analogy were carried to its logical conclusion,
it would help us deal with explosions
of hospitals with the death of all occupants. So, let’s
drop the airline analogy. It might be appropriate to think
of patients as baggage of different sizes and shapes, and the
challenge of medicine might be envisioned as the ability
to handle these well. We do better with the management,
delivery and safe-guarding of medications than the airlines
do with baggage. The handling of patients is a much a
larger and complex challenge.
“Quality improvement does not comport well with
patient experience. System error has displaced impairment
or incompetence of individuals. It is still true that
‘bad apples’ like Dr. Shipman in the UK require individual
responsibility, as a focus for management. Our
healthcare workers, a ‘vulnerable population’, are suffering
from safety program fatigue. New interventions to deal
with the challenges outlined in the Institute of Medicine
Report ‘To Err is Human’ include rescue teams, electronic
records for order entry, the 80 hour workweek and other
innovations. Fatigue errors are rare and, interestingly, the
80 hour workweek did not improve outcomes. 80 hours is
just 8 hours short of half a week, a long period of service.”
In Charles’s study of the 80 hour week, he found that
hospital computers were set so that they could not accept
more than 80 hours. This resulted in full compliance, an
imaginary accomplishment.
“Safety innovations have drained face to face interactions
and therefore have drained trust. Technology is
opaque, making problems difficult to identify and fix.
Interns involved in night float coverage,
a remarkably inefficient innovation of
the 80 hour workweek, go from a panel
of 10 patients during the day (3 sick, 3
safe, and 4 uncertain) to a panel of 60
patients as they cover 6 services on the
night float. That means 18 sick and 12
uncertain, an impossible assignment of
responsibility.
|
“System error tends to end the discussion
of most clinical errors. No one
feels responsible and there is no incentive
to solve system problems, which are
beyond individuals’ capability to change.
Similarly, checklists encourage mindlessness.”
In a gracious footnote, Charles
referred to his position as an observer and
commentator on the problems of surgery.
Quoting Mark Siegler, he said ‘I have the counterfeit courage
of the non-combatant’.
“Health is a public good that has been transformed
into a marketplace good. This creates a tension between
the ideal and the real. We need to correct the mistaken
assumptions embedded in policy solutions. Fools are
cleverer than system designers. It is difficult under current
dogma to determine what counts as a mistake.
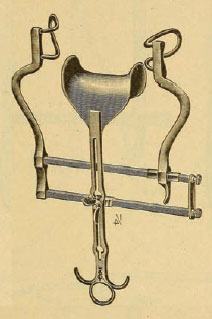
The Balfour retractor, for many years a
staple of abdominal surgery
“There is a lesson to be learned. The job of residents
is physically and cognitively demanding. Residents are
required to make decisions under time pressure, with
incomplete knowledge in the presence of uncertainty.
This leads to errors and adverse outcomes, but error is an
essentially contested concept. We cannot define it out of
context. Residents can only use tentative reasoning in the
presence of uncertainty. If A is true, then B may be the
best decision in this setting. [If A cannot be known at the
time a decision is required, defensible errors can follow.]
“We need to look at health policy on the street level.
The IOM Report of 1999 used an unfortunate model –
the body count model, where there are 44,000 or 86,000
or 98,000 deaths in the healthcare space caused by error.
The goal to cut the number in half by 5 years involved
technology, such as electronic order entry, the electronic
record, the 80 hour week, and various other system fixes.
The ‘To Err Is Human’ Report has led to ‘techno – vigilance’
in the United Kingdom, and technology solutions
in the United States. The solution is not more robots, we
need more discussion of surgical judgement.
“In medicine, death occurs related to the pathophysiology
of disease. In surgery, it does not result from the
pathophysiology of disease, because of surgical agency to
interrupt the pathophysiology. In medicine, when a patient
dies, colleagues ask: ‘What happened?’ In surgery, when a
patient dies, colleagues ask: ‘What did you do?’ The challenge
for the future is to align the experience of the patient
with the experience of the surgeon, and to curb the enthusiasm
of surgeons and patients for operations that defy the
odds and result in miracles. The value of the ‘time-out’,
even though it seems counterintuitive for each individual
to say their name prior to the surgical operation, is that it
enables people to speak when a later challenge occurs. We
need to punish those who do not speak out.
“In the post Greenspan era, we have been taught to think
differently about return on investment. Return to capital is
perceived as progress. Return to labour is seen as inflation.”
Charles’ goal is “engaging people’s understanding
of what they are doing”. He is an enthusiastic student
of the great sociologist Elliot Freidson, author of the
“Professionalism; the Third Logic”, a thought-provoking
critique of the notion that the market or corporate
structures like governments or institutions can provide
adequate logics or conceptual frameworks for civilization
to flourish. His Balfour lecture on Surgical Ethics
was a highly praised demonstration of the importance
of Professionalism as a guiding framework for addressing
important challenges faced by surgeons.
M.M.
|