Cognitive Dissonance
and Evidence Based
Medicine - David
Naylor’s Kergin Lecture
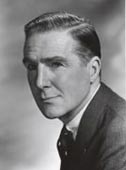
Frederick Gordon Kergin
|
Frederick Gordon Kergin
was born at Port Simpson
in British Columbia in
1907. He began his studies
at the University of
Toronto at age sixteen
and graduated from the
Biology and Medical
Sciences program in
1927. In 1931, Kergin
became a Rhodes Scholar
and spent the next two
years at Oxford University in a Master’s Degree program
in physiology and anatomy, graduating with
first-class honours. In 1934, he began the four-year
Gallie Course in surgery at TGH and obtained
the fellowship of the Royal College of Surgeons
of England in 1935 and that of the Royal College
of Physicians and Surgeons of Canada in 1939.
In 1937, he joined the surgical staff of Toronto
General Hospital and later took the role as Chair
of the Department of Surgery of the University
of Toronto and Surgeon-in-Chief of the Toronto
General Hospital from 1957 to 1966. He was a
pioneer of thoracic surgery in Canada and served as
President of the American Association for Thoracic
Surgery. In1966, he was appointed Associate Dean
in the Faculty of Medicine and was responsible for
developing a new undergraduate curriculum and
planning the conversion of Sunnybrook Hospital
to a teaching institution with full-time faculty. Dr.
Kergin chaired the editorial board of the Canadian
Journal of Surgery for many years and served as a
trustee of the R.S. McLaughlin Foundation.
His major contribution to the University was in
education, particularly in structuring the residency
programs such that an integrated program amongst
all fully affiliated hospitals was established. Professor
Kergin died in 1974, a man with eclectic interests
that included teaching, research and university
administration, as well as many outside of medicine.
(http://surgery.utoronto.ca/events/kergin-lecturers.htm)
|

James Rutka and David Naylor
The 2017 Kergin Lecture was delivered by David Naylor,
former Dean of the Faculty of Medicine and President
Emeritus of the University of Toronto. Naylor’s theme
was ‘Cognitive Dissonance and Evidence-Based Medicine’
[EBM]. Based on his studies of an American religious cult,
psychologist Leon Feininger coined the term ‘cognitive
dissonance’ in 1956 to designate the distress people feel
when reality conflicts with deeply-held beliefs. Cognitive
dissonance is resolved by denying, ignoring, or reinterpreting
the contradictory finding which does not fit with
our biases or beliefs. Naylor drew on his long experience as
a researcher and policy advisor to examine applied health
research, healthcare policy-making, and clinical reasoning,
all viewed through the lens of cognitive dissonance.
Starting with research, Naylor observed that clinical
epidemiology emerged in the 1970s and 1980s as a discipline
that aimed to enhance the rigor of clinical studies
and bring research results to bear more fully on clinical
decisions. These insights were synthesized and presented
to the profession in the early 1990s as ‘Evidence-Based
Medicine’ [EBM]. EBM was described as a new clinical
‘paradigm’, i.e. a system of assumptions, concepts, values
and practices that constitutes a way of viewing reality. It
characterized clinical experience as an unreliable source of
evidence – an apparent devaluation of clinical judgement
that understandably unsettled many surgeons given the
highly case-based nature of their work. Naylor observed
that, more generally, EBM as a paradigm has continued to
struggle with the dilemma of the applicability of evidence
and the unreality of the ‘average patient’. Small effects that
turn out to be statistically significant in giant randomized
trials mean that many patients are exposed to side-effects for
everyone who benefits from a given ‘evidence-based’ treatment.
EBM acolytes often argued that the solution was to
stratify subgroups of patients by baseline risk, assume the
same relative benefit would accrue to all, and therefore infer
that the highest-risk patients would gain the most in absolute
terms. However, studies using sophisticated biomarkers
are starting to overturn this mode of reasoning.
To illustrate this point, Naylor showed us a randomized
trial of the cardiovascular drug Dalcetrapib (Tardif JC et
al, Circ Cardiovasc Genet. 2015;8(2):372-82) that initially
found no difference when the drug was compared to placebo.
Use of biomarkers later revealed that the drug was
highly beneficial in one genetic subgroup and harmful in
another. The two effects cancelled, leading to an erroneous
‘evidence-based’ conclusion. Naylor suggested that this
result was a bellwether for the challenge facing the current
incarnation of EBM as ‘the medicine of averages’. He
observed that a counter-paradigm was emerging as biomolecular
characterization of patients continued to advance,
thereby enabling better tailoring of treatments. He predicted
that new molecular markers and other measures such
as functional imaging were likely to compel reconsideration
not just of who received specific treatments, but how we
define disease entities, particularly in disciplines such as
psychiatry, with its descriptive Diagnostic and Statistical
Manual of Mental Disorders (DSM).
Naylor emphasized that consideration of variations in
patient characteristics and anticipated responses to treatment
has been an integral part of expert judgement dating
back centuries in clinical medicine. What is different
now is the convergence of our deepening understanding
of human biology with other factors such as the use
of digital devices to enable continuous monitoring of
patients with sophisticated sensors, improved imaging,
automated treatments based on digital monitoring and
the application of artificial intelligence. Sophisticated
tissue engineering techniques may transform not just
the field of transplantation but surgery in general. This
layering of diverse disruptive forces has meant that the
once-popular term, ‘molecular medicine’, is already
being largely supplanted by terms such as ‘personalized’
or ‘precision medicine’.
|
Just as the emergence of EBM seemed to engender
cognitive dissonance among those attached to other
modes of thought and action, so also was it now ironically
the case that EBM fundamentalists were among
the most vocal critics of personalized or precision medicine.
Naylor cautioned, however, that personalized or
precision medicine was far from a panacea. It had the
potential to provide remarkable improvements over the
“shot-gun approach” of EBM, but many exaggerated
claims were already being made for this latest paradigm
and the potential costs and risks are enormous.
Other countries such as the UK and Australia were
more enthusiastic about precision medicine, and more
thoughtful about developing a reliable knowledge base
and strong framework for funding and using these
concepts in practice. Developing a Canadian national
strategy for personalized medicine was accordingly
among the recommendations made in 2015 by a distinguished
Advisory Panel on Healthcare Innovation that
Naylor chaired for the federal government (link to PDF). Although the Conservative Government
of the day shelved the report, it has found new life under
the current Liberal Government, underscoring Naylor’s
comment that political ideology of all types carries its
own forms of cognitive dissonance. Naylor among others
who promoted EBM in the 1990s had emphasized
that clinical decisions would continue to rest not only
on evidence, but on a given patient’s values or preferences
and the context of the clinical encounter (Naylor
CD. Lancet 1995; 345 (8953):840–2). He wondered if
that list should now be expanded to include cognitive
psychological factors, and particularly in the realm of
healthcare reform, overtly political or ideological considerations.
In support of that point, Naylor reviewed some work
from his early years at the Institute for Clinical Evaluative
Sciences (ICES), showing remarkable variation in rates
of caesarian sections, hysterectomy, knee replacement,
and breast conserving operations. This work had caused
a media sensation when it first appeared in 1994.
Politicians were quick to criticize the profession; physicians
and surgeons in turn rushed to explain away the
variations in very creative ways.

Naylor emphasized that while some practice variations
reflected indefensible departures from rigorously assessed
practice standards, in other instances they reflected
evidentiary uncertainties, different financial and organizational
contexts, and regional or national clinical
cultures. On the latter point, he reminded the audience
that expert panels from different countries would arrive
at different views about the appropriateness of surgery
when given the same evidence and patient case scenarios.
Naylor then showed real-world examples of this phenomenon
in the realm of differences between Canadian
and American practice patterns in use of cardiovascular
procedures after myocardial infarction (Mark DB et al.
N Engl J Med 1994; 331:130-135).
Naylor also summarized several studies led by Toronto
researchers illustrating how errors in cognitive processing
affect decision-making. For example, physicians were
more likely to favour testing and treatment when considering
their recommendation to an individual patient than
when they were asked to consider how they would write
guidelines for a group of similar patients (Redelmeier
DA, Tversky A. N Engl J Med. 1990;322:1162-4). The
framing of treatment data also has a powerful effect. A
new drug might reduce death rates for a given condition
from 4 per 100 patients treated to 3 per 100 -- a 25%
relative risk reduction. However, if the same data are
shown as a 1% absolute reduction, or represented fairly
by the statement that 100 patients must be treated with
the drug to save one life, then physicians become much
more cautious about recommending the new medicine
(Naylor CD, Chen E, Strauss B. Ann Intern Med.
1992;117(11):916-21).
As a final example of how politics and cognitive dissonance
can shape the use of evidence, Naylor pointed
out that in the early 1980s a rigorous randomized trial
undertaken by RAND researchers had shown that costs
were lower and outcomes similar with a comprehensive
capitated plan (then known as an HMO and now more
commonly termed an integrated delivery system) as compared
to Canadian-style health insurance (Manning WG
et al. N Engl J Med 1984;310:1505-15). The findings had
limited uptake in the US due to lobbying by organized
medicine and the private insurance industry, and were
downplayed here because of smugness about Canada’s
superior healthcare system and physician unease about
changes in compensation modalities. In part because of
our refusal to embrace such changes, the performance of
Canada’s healthcare system is now seen by many experts
as lagging behind a number of OECD peer nations.
Naylor closed the Kergin Lecture with two aphorisms
that encapsulated his theme of cognitive dissonance and
evidence-based medicine/policy-making. The first was
from a collection of essays on medical history published
in 1991: “The enduring lesson of history may be that
social change is inevitable and institutional progress possible,
but human nature is wonderfully intransigent” (1).
The second, arising from three decades of experience
as reflected in the lecture, was shorter: “How we think
is more important than what we know --- or think we
know”.
(1) Naylor CD, ed. Canadian Health Care and the State. Montreal:
McGill-Queen’s University Press, 1992, p12. |