Palmer Lecture: Surgical Treatment of the Obesity Epidemic

Aurora Pryor
|
The 2010 Palmer lecture
was given by Aurora Pryor,
Associate Professor of Surgery
at Duke University Medical
Center and co-Director of the
Duke Metabolic and Weight
Loss Surgery Program. Aurora
received a biomedical and electrical
engineering degree at
Duke University and subsequently
completed her medical
and surgical training there. She is Chief of General Surgery at Durham Regional Hospital, an inventor, a
teacher, and an expert in bariatric surgery.
|
John Angus Palmer completed the Gallie Course in
General and Plastic Surgery in Toronto and fellowship
training at the University of Edinborough and
St Marks. He was a master surgeon, an astounding
technician, a thoughtful clinician and gifted teacher. His
expertise covered a very broad range of general, head
and neck, endocrine and cancer surgery.
John had numerous and eclectic interests outside of
surgery: his family, painting, collecting art, collecting and
refinishing antiques, carving decoys, anatomy, skiing and
boating, to name a few. He also mixed a mean pitcher
of martinis. As a centennial project in 1967, he and his
family dismantled a pioneer log house and reconstructed
it near their family cottage in Dwight, Ontario. They
then opened it to the public as a charming antique shop.
Lorne Rotstein
|
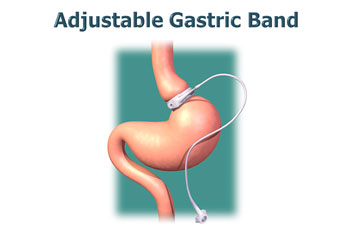
Aurora first documented the obesity epidemic in
North America, then explained that there are two classes
of operative treatments for obesity - restrictions and
diversions. Gastric restrictions use adjustable bands or
sleeve reduction to create a sensation of fullness after
the residual small gastric pouch is filled. Afferent vagal
fibers from the proximal stomach that remain in continuity
transmit a message of satiety after only a small
meal following these procedures. Combined diverting
procedures involve some re-routing of the gastrointestinal
tract. These procedures, including Roux -en-Y
reconstruction or a duodenal switch are more complex,
but offer a more reliable rate of sustained weight reduction.
She favors the Roux-en-Y procedures because of the
dramatic cures of diabetes - powerful evidence that is evident
even a day or two after surgery. (Perioperative Safety
in the Longitudinal Assessment of Bariatric Surgery, N
Engl J Med 2009; 361:445-54). John Palmer performed
the first bariatric surgical procedure in Canada as one of
his many innovative contributions. The operation was a stapled gastric restriction procedure.
 |
 |
|
Among the 3,500 bariatric operations performed at
Duke (600 procedures per year), 17% are restrictive
operations and 81% are diversions. There is a 70%
long- term stable weight loss rate with the Roux-en-Y
procedure. Associated with that weight loss is significant
reduction in medical co-morbidities associated with obesity,
such as diabetes or hypertension. Overall the 30-day
mortality of primary bariatric surgery in the Duke series
is 0.25%. In a large series followed at McGill University,
comparing surgery with medical care in obese patients,
the five year mortality is 0.68% in patients treated surgically
and 6.17% with medical care alone. The benefits
of surgery are striking: 76.8% complete resolution of
diabetes and 86% improvement in control of diabetes.
Blood pressure is reduced, hospitalizations are reduced,
return to work among disabled morbidly obese Medicaid
patients is 37%. Complications include anastomotic leak, thromboembolism and marginal ulcers.
Steps to reduce the risk of surgery include careful
anticoagulation, preoperative weight loss and blood pressure
control. All patients are treated with proton pump
inhibitors, as the incidence of marginal ulcers was 4.7%
in the initial series. One of the complications of restrictive
operations using adjustable bands is slippage of the band in 5-10% of patients.
Centers of excellence in Bariatrics are becoming more
widespread in the United States; they are required by
many insurance payers in order to qualify for reimbursement.
A large centre such as the Duke Centre provides a
stable team of caregivers including psychologists, nurse
practitioners, dieticians, surgeons and dedicated operating
teams. Such centres require devotion of considerable
operating time and space to the program.
The University of Toronto Bariatric Program will use
a more distributed hub and spoke model. There will be
one central program but the operations will be distributed
(New Bariatric Surgical Program Established at University of Toronto, The Surgical Spotlight, Spring 2009).
During a spirited and well-timed discussion period,
Jack Langer asked about the use of bariatric surgery in
children. The Duke program is just starting a paediatric
program; there are important questions about the effect
of the operation on development to be answered from
experience.
Andy Smith asked about warning labels, analogous to
those on cigarette packages. The widespread use of high
fructose corn syrup in many foods and the supersizing of
commercially available portions present a health hazard.
Labeling has only begun to be practiced, but warning
does not yet appear on packaging. Richard Reznick
asked about non-surgical interventions - apparently
there are endoluminal sleeves that can be introduced
by gastroscopy and gastric balloons to fill the stomach.
Experience with these is very preliminary.
David Urbach asked about the best way to develop
a program. Aurora felt that starting with simpler operations
to develop proficiency and good results had been
helpful at Duke. Kyle Anstey asked about performing
bariatric surgery in developmentally or cognitively
impaired patients. Because of potential problems with
management in the longer term, Aurora recommended
that accepting these patients for surgery be delayed until
the program is better developed.
Allan Okrainec asked about surgery in the elderly.
Duke has no cut off, but the province of Ontario has
recommended that surgery be offered only to those who
are under 60 years of age. There is not yet sufficient
experience to know how valuable the surgery will be in
non-obese diabetics. It is interesting to note that gastric
surgery, once a very significant part of general surgery
practice, has been eclipsed in recent years because of
effective pharmacotherapy for peptic ulcer and reflux
disease. The obesity epidemic has returned gastric surgery
to a prominent place in surgical practice.
M.M.
|