International Surgery: Challenges and Responses
"Most people on the planet who need surgery can't get it.
Changing this surprising situation is a challenge to which
universities should rise - to solve the problem or to train
people who can solve it. As an academic health science
faculty, we cannot provide health care for Canada, much
less the world. We don't build healthcare infrastructure, but
what we can provide is training." - Andrew Howard
In 1999, John Wedge and Massey Beveridge founded the
International Surgery Office within the Department of
Surgery, and Andrew Howard joined the enterprise. He
now serves as Director of the Program. Andrew has had
a long interest in surgical education and surgical care
in Africa. He has a mandate to study injury control in
African children. In this resource constrained setting, the
infrastructure required for care and research is severely
limited.
There is a long and distinguished history of Canadian
participation in International Surgery, dating back to
Norman Bethune, a University of Toronto graduate
and hero of International Surgery in Spain and China
Canadian Cardiac surgeon Lee Erett won the Norman
Bethune award from the Chinese Government for operative
teaching and practice in China (see also http://www.surgicalspotlight.ca/Shared/PDF/Spring07.pdf ). For
many years, our surgeons have been going to where they
were needed and treating grateful patients, regardless
of their ability to pay. Readers will be familiar with the
problems of HIV, tuberculosis and malaria in Africa, but
there is a less well-known problem- the severe deficiency
of surgical care. 13% of Africans die from trauma and 1
in 13 women die in childbirth.

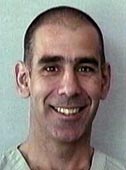
Andrew Howard with his wife, Lianne and their two daughters, Emma
and Samantha
The service needs overwhelm capacity. There are
only 400 surgeons in all of East Africa. Most are very
busy. They do private work to support themselves and
provide care in the public system, leaving little time
and no financial support for teaching. The University
of Toronto psychiatry program led by Clare Pain provides
a very effective model. They have worked with
psychiatrists at the Addis Ababa University in Ethiopia.
Ten years ago, there were no residents. They now have
a functioning residency and have raised the number of
practitioners in the country from 3 to over 3 dozen.
Based on this example, Ted Gerstle is developing a similar
program in pediatric surgery, and Andrew is trying to
do the same in Orthopaedic surgery.
The Office of International Surgery provides electronic
access to the University of Toronto library, so surgeons
and other healthcare personnel in Africa can share
our textbooks, journals and other subscription- based
services. The librarians who have made this possible
are Sandra Kendall at Mount Sinai Hospital, and Sian
Meikle and Warren Holder at the Robarts Library. The
Office of International Surgery provides the services to
several hundred surgeons in Africa and supports librarians
in Africa to facilitate their use.
The College of Surgeons of Eastern, Central and
Southern Africa (COSECSA) is a certifying body that
has developed surgical training programs (see also http://www.cosecsa.org/). The College approves training by
skilled surgeons at busy community hospitals as well as
university sites. There is an online course with a tutorial
to help candidates pass the College exams (see http://www.ptolemy.ca/members/). The entries are developed
by African surgeons in combination with a Canadian
author to provide an international perspective. Some
of the work on this project has been published in the
Canadian Journal of Surgery. The training process is
somewhat like the British system. There is an early
exam, analogous to the British Fellowship exam or our
Principles of Surgery Exam, followed by specialty-specific
training in various disciplines such as paediatric surgery,
urology etc. Canadian surgeons provide examiners,
but also develop curricula and travel to Africa as teachers.
When I interviewed Andrew, he had just returned
from giving exams in Uganda for COSECSA.
Andrew was born in Edinburgh, grew up in High Prairie
Alberta, completed his undergraduate medical training
and surgical residency at Queens, followed by a fellowship
in Orthopaedic Surgery at the Hospital for Sick
Children. His wife Lianne and two daughters Emma and
Samantha accompany him on his paddling and skiing
forays into the Canadian wilderness, and they are looking
forward to travelling to Africa together one day.
The Office of International Surgery has brought surgeons
to Toronto to study. For example Milliard Derbew
spent a sabbatical year at the Wilson Centre, studying
Surgical Education (see also the Surgical Spotlight, Spring
2006, page 9, or go to http://www.surgicalspotlight.ca/Shared/PDF/spring06.pdf). He subsequently became
Dean of Medicine at Addis Ababa University. There is a
striking need for paediatric orthopaedic surgeons in Africa,
given that almost half of the population is less than
15 years old. Andrew's hope is to develop a Canadian
Community of Interest in Surgery in Africa. "We are at
a very early stage, but the Surgeon Scientist and Surgical
Education Program grew from a small group of interested
surgeons to major themes in our department."
|
UNIQUE APPROACHES TO THE CHALLENGE

Alex Mihailovic
|
Alexandra Mihailovic is a Critical Care fellow who
completed our general surgery residency with a focus on
trauma. Her critical care program includes 13 months of
core training in various disciplines, including transplantation,
medicine, surgery, and seven months of trauma
training in Cape Town.
The experience in Cape Town is enlightening and
intense - four to five thoracotomies or laparotomies per
day, largely for gang - related injuries in the townships -
"When a patient has been shot and there are 4 bullets on
the chest X-ray, it's impossible to tell which are today's
bullets. It's difficult to record outcomes in this population
as most of the patients will never return for follow
up once they've left hospital. The sanctity of life is less
cherished. When a 22- year old dies in the operating
room, the staff comforts the surgeon saying: 'He probably
killed five people today before he was shot'. Some
staff are resentful of putting
multiple units of 'our blood
into this killer'."
Alex worked with Neil
Lazar in the medical ICU
at UHN. She became very
interested in ethics and social
determinants of illness. "In
Africa, there is little investment
in prevention of trauma
and therefore no reduction
in the cost of patching up the surviving victims." Alex is
a PhD candidate, studying the epidemiology of trauma
in Uganda. Andrew Howard is on her committee. She
also spent two months in Haiti, as the only surgeon at
the time she was there, treating victims of the earthquake
and the results of displacement post earthquake with the
Canadian and German Red Cross.
One of the striking problems in Haiti was the intervention
by doctors from NGOs, who performed elective
operations in addition to emergency care. This was
encouraged by many NGOs, because they provide the
opportunity for publicity photos. However, diverting
patients to a free elective surgical service deprives the
local surgeons of the fees they need to buy food and
maintain their lives in Haiti. "There is a danger that
NGOs might eventually force the local doctors to move
to Miami or elsewhere in order to make a living. I felt
more like a culprit in this situation, as the local doctors
said: 'I can't feed my children if you visiting surgeons do
the hernias, gall bladders and cesarean sections'."
Alex found a middle ground, debriding ulcers, rotating
flaps, treating burns, operating only on inpatients
and emergency cases to keep her out of the elective
schedule. The ethical quandary after surgery is - "where
do these burned patients and paraplegic patients go?
People in wheelchairs can't travel where there are no
roads and often there are no rehabilitation or prosthetic
services available to help them gain independence
again...so after all that work to get them surgically
healed you then are left with a patient you can't discharge
into the streets."
Georges Azzie
|
HSC surgeon Georges Azzie focuses his practice of
international surgery in a setting where he was initially
employed by local authorities (Botswana) and
where he knows and understands the environment.
Programs he has helped foster
are based on local needs
assessments. Georges helped
develop a multi-facetted program
to develop laparoscopic
skills among surgeons. This
included (but was not limited
to) yearly workshops, a
telesimulation program done
in conjunction with Allan
Okrainec (see also Surgical Spotlight Winter 2009) and ongoing support at multiple
levels. [There is an interesting response to this
important contribution to international surgical education:
Some program directors from higher income
countries object to teaching minimal access techniques
to local surgeons. They send their residents to Africa to
perform open operations as surgical tourists. "Where else
can they get this experience?" - Ed]
Georges' experience leads him to minimize the
destructive side - effects of "surgical tourism" in low
and middle income environments. He is "the first to
admit that he has more questions than answers with
regard to addressing the global burden of surgical
disease and to mentoring those with similar career
interests."
|
The 11th meeting of the Bethune International
Surgery Round Table will be held in Montreal,
June 3rd, 4th and 5th 2011 (http://www.cnis.ca/what-we-do/public-engagement-in-canada/bethune-round-table/). Eight of the previous meetings
have been held in Toronto. The round table draws
surgeons from Canada, South America, South East
Asia and elsewhere to teach and learn about international
surgery.
|
M.M with notes from Andrew Howard,
Alexandra Mihailovic and George Azzie
|