An Intestinal Operation Can Cure Diabetes
A laparoscopic Roux-y operation cures diabetes in
70-85% of obese patients. "Cure" means a normal
hemoglobin A1C and no medications, with normal
glycemic control.
Working with a team of nurse practitioners, social
workers, psychiatrists, internists and dietitians, surgeons
in Toronto have been developing an integrated bariatric
surgery program that is having remarkable success in
controlling diabetes. Patient access to the group comes
through the Ontario Bariatric Network, a web-based
referral system. The typical patient has a body mass
index (weight in kilograms divided by height in meters
squared) of 40 or higher. Only 20% are men, a self-selection
bias. Patients have various co-morbid conditions in
addition to diabetes- many have sleep apnea, hypertension,
various musculo-skeletal syndromes, and psychological
troubles including depression and physical abuse.
Patients are referred to the Bariatric network through
their family doctor. They see one of the nurse practitioners
first and then attend a group education seminar.
They then undergo sleep studies and are screened metabolically
for compliance with smoking cessation. The
patients see the surgeon last after thorough screening
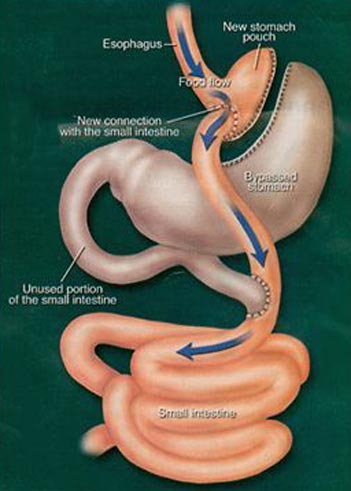
and conditioning by the bariatric team. The operation
of choice is the Roux-y bypass. Though it is done widely
in the community, gastric banding is not part of the
practice, and vertical sleeve gastrectomy is used in only
5% of patients. There is an 85% success rate in the early
experience. The program is intended to provide surgical
care for up to 400 patients per year. The surgeons are
careful to stay off social networks, as there is considerable
exchange of detailed information
among patients who
are seeking bariatric surgery.
"Sometimes consumerism
and vanity clash with fidelity
to the values of our profession.
Much of the information
that is exchanged is too
good to be true or misleading.
‘I want a 34 French bougie
sleeve resection’ is a challenging
way to start a conversation."

Todd Penner
|
Todd Penner describes the dramatic change seen in
patients following surgery. "They come the post-op clinic
with new clothes, their hair redone, new dental work
and they can’t stop smiling. The patient who came in on
Metformin and 100 units of insulin is off medications
in 5 days with normal glycemic indexes. The metabolic
effects are absolutely dramatic and not strictly related to
weight loss. Obese patients are stigmatized in society and
are often desperate for relief from their social discomfort.
Healthcare personnel were initially participating in this
stigmatization. The ‘you did it to yourself ’ bias is finally
going away as the program advances. "
Our surgery is resource intensive, as we cost the
hospital $3-4,000 per case for staples and instruments.
Bariatric surgery is volume funded, so the Ministry of
Health has an important controlling effect on practice
through the hospital CEOs. There are advocacy groups
that also influence practice.
|
Todd describes himself as a common operations general
surgeon and a teacher rather than a researcher. He is
proud of the SAGES - accredited fellowships the group
has established, allowing training of three surgeons per
year. "We have a great simulation lab here at Toronto
Western Hospital and we are creating a Canadian cadre
of bariatric surgeons."
Todd has won many teaching awards including
the Ross Fleming and Frank Mills Award. He is currently
reading Physician-ethicist Carl Elliott’s ‘White
Coat, Black Hat", a description of bodily enhancement
through surgery.
With his wife Shelley, a fitness model, nurse and
mother of two, Todd is very active in running. They have
both completed the Chicago, New York, San Francisco,
Ottawa and Toronto marathons.
Allan Okrainec completed a minimally invasive surgery
fellowship in Montreal. Tim Jackson did his in Boston and
David Urbach at Portland, Oregon. Todd Penner’s fellowship
was with Lloyd Smith in Toronto. All of the surgeons
were locally mentored by John Hagen at the Finch site of
the Humber River Regional Centre. "John mentored us for
the first 10-20 cases. We went up to his operating room
4-5 times, then he came down, then we worked together
in pairs on easier cases, then moved on to the harder ones.
Males in general are much more challenging to do than
females, as female fat is deposited outside the fascia. Men
put it inside. With thin arms and legs, they have massive
abdominal and retroperitoneal fat. They need the surgery
more for the metabolic effect, but the driver of cosmesis is
not as strong in men. It is a good ethical issue as we could
help men more metabolically. The surgery is exponentially
harder to do in men. The liver, especially the left lateral segment
is massive. We shrank their livers on Optifast, which
makes 25 to 50% of the liver go away."
M.M.
Commentary on Bariatric Surgery

John Hagen
|
"We do not know why
men are shaped like
apples and women are
shaped like pears, but the
intra-abdominal fat distribution
in obese men
makes bariatric surgery
very challenging. The
reason that the operation
works metabolically may
be related to the delivery
of undigested food into the small bowel. The
intra-abdominal fat is reduced pre-operatively
by having the patient take a 900 calorie diet of
Optifast, five packages per day -high protein, low
fat, low carbohydrate and appropriate vitamins.
The liver is the first place to lose weight, then
visceral fat in the omentum, retro-peritoneum
and mesentery. The Optifast technique is being
used for facilitating other intra-abdominal surgery
than the gastric bypass. For example, it is
currently used for colon cancer surgery."
There are four bariatric programs in Ontario - one
in Ottawa, one in Guelph, one in Hamilton
and one in Toronto. The Toronto program is
comprised of the Humber River Hospital, St.
Joseph’s, Toronto East General Hospital and
Toronto Western. Residents and fellows rotate
at the Humber Hospital as part of the general
surgery program. The cases are expensive in that a
lot of staples are used, but the funding is volumebased
on a special budget from the Ministry of
Health. The cost of the operation is recouped in
three years from the cost- saving for drugs that
the patients no longer need for their diabetes,
hypertension and hypercholesterolemia.
Although we quote a 30 day mortality of 1
in 200, across Ontario the mortality rate is less
than 1 in 1000, which is similar to the mortality
rate of laparoscopic cholecystectomy. Patients
can develop complications including internal
hernias and malabsorption, so they are required
to take certain medications for life, including
iron, calcium, thiamine, folic, B12 and vitamin
K. If they don’t agree that they will take these for
life, they are not given an operation."
The future for this form of surgery looks like
one of increasing demand and increasing expansion.
[the day of this interview, John was going to
Sick Kids Hospital to help the surgeons perform
bariatric surgery on an obese child.] "Success will
come as the general populus becomes more aware
of the success of the operation. There are estimated
to be 160,000 people in Ontario with the
body mass index of greater than 40, the threshold
for surgery. We do 2,700 cases a year."
M.M.
|
|